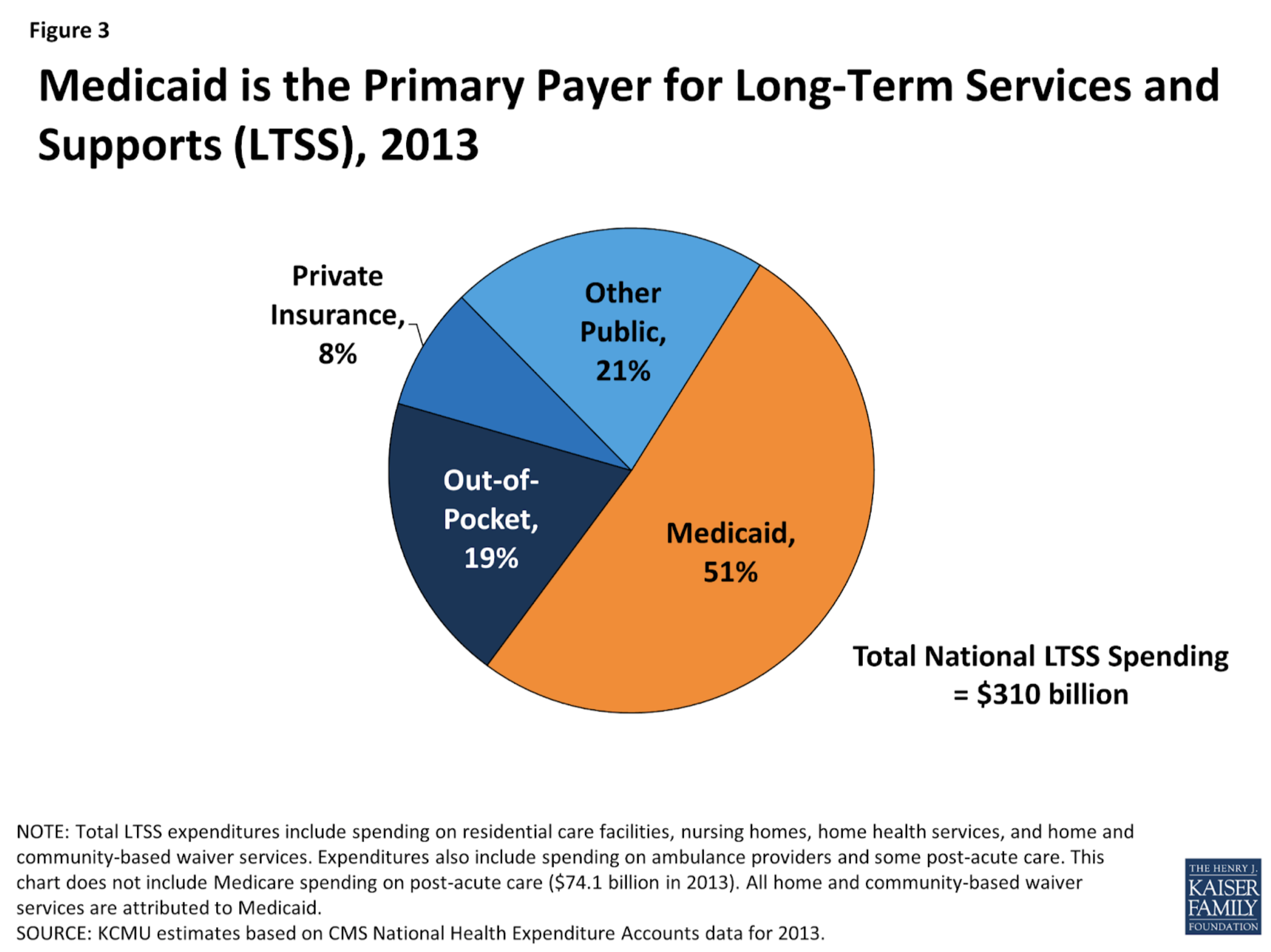
Most people ages 65 and older and many people under age 65 with disabilities have Medicare, but Medicare does not cover most LTSS. Instead, Medicaid is the primary payer for LTSS. On this episode, we discuss the cost and coverage of Long term Services and Supports (LTSS).
The recent biennium budget approval is allocating additional funding to those Administrations which provide Long Term Services and Supports: ALTSA & DDA. In the coming weeks, as the state is synthesizing the budget details, Washington’s Medicaid delivery of LTSS will be planning for implementation and operationalization in the new fiscal year-which begins July 1. Some of the highlights which WA will be planning for are:
- Home care worker shortage LTC workers
- Changes to family member definitions
- Pilot for paid spousal personal care
- Savings from reduced training costs for family member IPs
- Community Housing Transitions
- Interim slots, landlord retainer payments, rental subsidies, behavioral health wraparound svcs
- $3M total when including savings assumptions
- Assume savings in federal dollars (?)
- Rapid Response Teams through FY24 (first year of biennium)
- $35M
- Behavioral Health Community Capacity
- More ESF and Specialize Dementia beds
- $30M
- Provider rate increases
- Nursing Homes – $219M, including specialty rate increases
- ESF – $16M
- Specialty Dementia Care – $22M
- Assisted Living – $117
- Nursing Services – $674,000
- CDE for IPs (and agency provider parity and AP admin rate increase) – $539M
- AFH bargaining agreement – $294M
- Kinship Navigator
- $2.5M
- LTSS (WA Cares) operations and IT
- $26M
Episode Sources:
- Conference Proposal Statewide Summary – 2023-25 Omnibus Operating Budget (wa.gov)
- Medicaid Home and Community Based Services for Older Adults with Disabilities: A Primer (justiceinaging.org)
- https://ofm.wa.gov/about/news/2023/03/state-revenue-projection-2023-25-forecast-decreased-483-million
- https://justiceinaging.org/wp-content/uploads/2021/04/HCBS-Primer.pdf
- https://www.dshs.wa.gov/altsa
- For further information on budget and coverages please visit https://www.dshs.wa.gov/altsa/long-term-care-services-information, and https://ofm.wa.gov/about/news/2023/03/state-revenue-projection-2023-25-forecast-decreased-483-million .
Podcast: Play in new window | Download